Introduction
Globally, including China, there is a resurgence of syphilis.1,2 This is especially marked in certain high-risk populations; for example, men who have sex with men (MSM) and heterosexual male and female drug users.3 I have increasingly been consulted on the interpretation of the various diagnostic tests, both now in private practice and previously in the public sector. This article will help you in selecting appropriate tests for screening your patients and interpreting the results.
Stage definitions for syphilis
Early syphilis:
- Primary: Patient may present with a painless chancre at the site of inoculation. Often asymptomatic, but multiple painful anogenital ulcers may also occur.4
- Secondary: Occurs in about 25% of patients with untreated primary syphilis. Clinical features may include: a mild nonpruritic rash, particularly on the palms and soles; lymphadenopathy; fever; mucosal lesions (eg, mucous patches or condyloma latum); alopecia; and occasionally hepatitis or nephritis.
- Early latent syphilis (ELS): Asymptomatic infection with syphilis, diagnosed serologically, within the first year after infection
Late syphilis:
- Late latent syphilis (LLS): Asymptomatic infection with syphilis, with time of infection greater than 1 year (or unknown).
- Tertiary: Includes cardiovascular disease (aortitis) and/or cutaneous gummas and/or neurosyphilis.
Syphilis may be sexually transmitted in primary or secondary syphilis and can be transmitted through blood transfusion potentially at any stage.
Type of syphilis serological tests
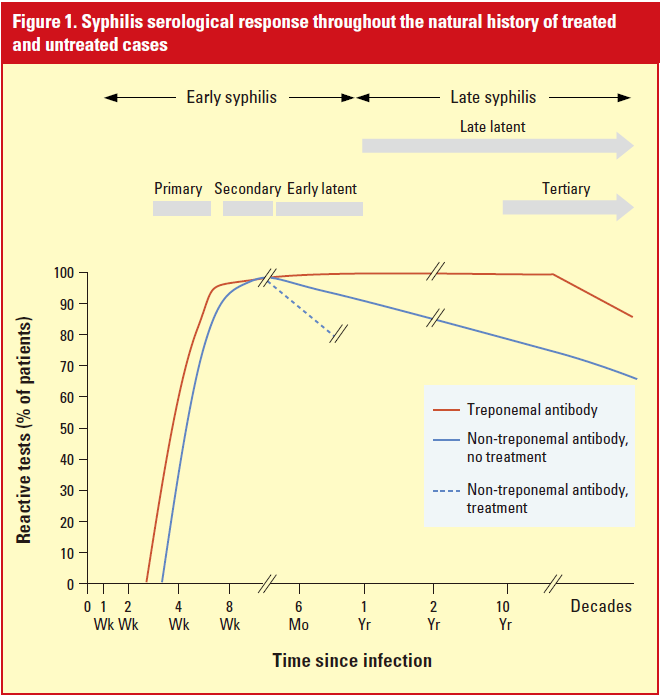
Diagnosis is made serologically via treponemal and non-treponemal tests as shown in the Table. Figure 1 shows the serological response of the two tests over different stages of syphilis.1
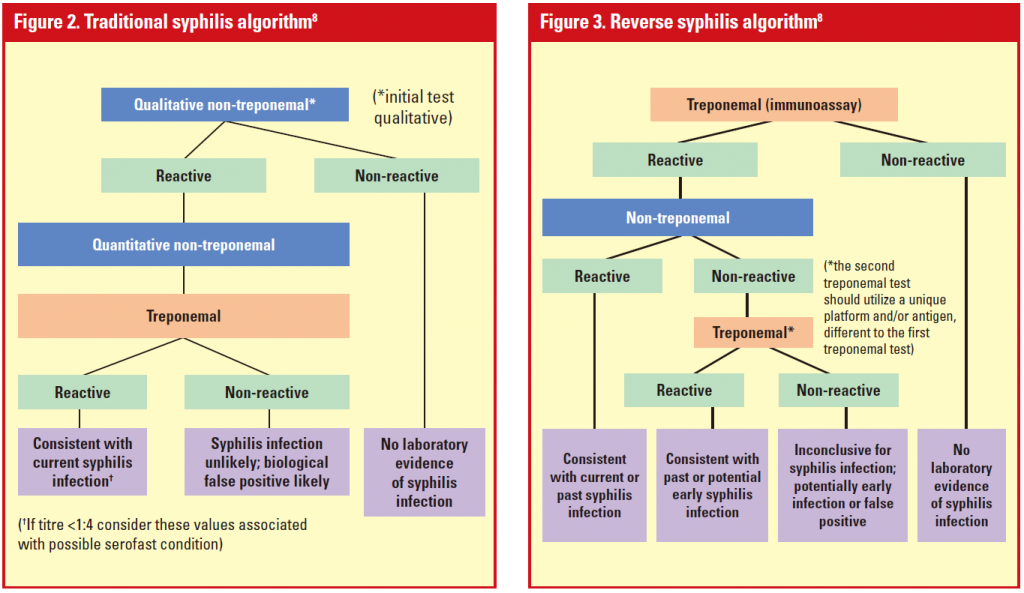
Testing algorithms8-11
The traditional algorithm screens patients using the non-treponemal test first, followed by the treponemal test for confirmation in a two-stage approach (Figure 2).
The reverse algorithm screens first with a treponemal test, such as T. pallidum enzyme immunoassay (EIA), an automated test that makes the process less labour intensive, followed by a non-treponemal test done reflexly to provide the titres that are necessary for clinical management (Figure 3). If the nontreponemal test is negative, an additional treponemal test, such as T. pallidum particle agglutination assay (TPPA), is usually done for further confirmation. The second treponemal test should use a different platform or antigen to the first treponemal test. Among the treponemal tests, the fluorescent treponemal antibodyabsorption (FTA-Abs) test is becoming obsolete because it is time-consuming, expensive and difficult to read. The T. pallidum haemagglutination assay (TPHA) and TPPA are inexpensive and widely used, but they are performed manually and subject to variation in interpretation between individuals. EIA/ELISA and chemiluminescence immunoassay (CIA) tests are typically automated but many remain expensive.12
Advantages of the reverse algorithm
- Early disease: Non-treponemal tests take time to become positive in primary syphilis. Therefore, screening with a treponemal test will be more sensitive.
- Late disease: With time, the nontreponemal tests may read negative in patients with untreated latent syphilis. Screening with non-treponemal tests only may miss some of these cases, especially in high-risk populations.
- Treponemal EIA is increasingly used as a first screening test based on the reverse algorithm due to the high throughput possible with automation. However, the test’s positive and negative predictive values for screening syphilis depend on the prevalence of syphilis in the population.
Table.Characteristics of syphilis diagnostic tests | ||
Test types | Treponemal Non-treponemal | |
Examples | EIA, TP-CL, TPPA, TPHA, FTA-Abs | VDRL, RPR, TRUST |
Reported as | • Reactive or non-reactive | • Titres (eg, positive in undiluted serum, 1:2; 1:4, 1:8, 1:16, 1:32, 1:64, etc) |
Detects | •Syphilis-specific antibodies | • Antibodies to cellular components (a cardiolipincholesterol- lecithin antigen) released during tissue damage caused by syphilis |
Changes over time | • Once positive, will remain positive for life | • With treatment, titres decline rapidly |
Uses | • NOT useful for distinguishing past from new infection and, hence, useless for following treatment | • Used to monitor response to treatment |
False positive | • Endemic treponematoses (yaws, bejel, pinta), other infections caused by spirochetes, eg, Lyme disease, mononucleosis, leprosy, malaria, systemic lupus erythematosus | Lyme disease, leptospirosis, Borrelia, leprosy, tuberculosis, pneumococcal pneumonia, endocarditis, rickettsia, |
False negative | • Rare | • ‘Prozone phenomenon’ can occur in 2% and appropriate dilution should be made if the index of suspicion is high |
Primary syphilis pretreatment | • 76%–96% positive (depending on tests used; FTA-Abs has lowest sensitivity compared with other methodologies)6,15 | • 78% positive |
Primary syphilis post-treatment | • Usually remains positive | • Four-fold decrease in titre is evidence of adequate treatment |
Secondary syphilis | • 100% positive | • 100% positive (titre usually reaching 1:32 or more) |
Secondary syphilis post-treatment | • Remains positive after treatment | • Four-fold decrease in titre is evidence of adequate treatment |
Latent syphilis pretreatment | • 100% positive | • 95% positive |
Latent syphilis post-treatment | • Remains positive after treatment | • Four-fold decrease in titre is evidence of adequate treatment |
Tertiary syphilis pretreatment | • 94–96% positive | • 71% positive |
Tertiary syphilis post-treatment | • Remains positive after treatment (if positive to begin with) | • Four-fold decrease in titre is evidence of adequate treatment |
Neurosyphilis diagnosis | • A negative treponemal test in CSF indicates that neurosyphilis is highly unlikely7 | • Best diagnosed by VDRL in CSF |
Currently, laboratories are increasingly adopting automated treponemal tests for screening. Public Health England13 and the International Union Against Sexually Transmitted Infections8 both encourage the use of a reverse algorithm that begins with a treponemal assay. As an initial screening test, a treponemal test is usually more sensitive in detecting very early syphilis compared with screening via a non-treponemal test. However, it can also result in a high number of false positives (ie, very low positive predictive value) in low-prevalence populations. For example, in low-prevalence areas, the negative predictive value of the treponemal EIA exceeds 98%; however, the positive predictive value is as low as 12%.14 In contrast, among higher-risk populations (eg, patients with other sexually transmitted diseases, including HIV), the positive predictive value can be as high as 90%.14
3 real-life cases
1. A 50-year-old, local, heterosexual man recently presented to my clinic with extreme anxiety concerning a recent ‘positive’ sexual health screen. He claimed his only sexual partner since marriage 20 years ago was his wife. Their sexual activities were unprotected. He had a history of gonorrhoea that had been treated more than 20 years ago. He could not remember whether he had had syphilis serology checked then. On this occasion, he had no specific genital symptoms. His sexual health screens, including urine and blood tests (HIV included), were all negative except for a positive treponemal EIA. The VDRL was non-reactive. The laboratory performed another treponemal test (TPPA) for him, which was also positive. He did not recall any genital ulcer or rash, and he had never been specifically treated for syphilis. LEARNING POINTS: This case illustrates the flow of investigations using the reverse algorithm. Further management would depend on the degree of suspicion for neurosyphilis. As treatments for neurosyphilis and late latent syphilis differ, some specialists would elect to do a lumbar puncture whereas others would treat this as late latent syphilis if the likelihood of neurosyphilis is sufficiently low. |
2. A 33-year-old Chinese lady was referred because she screened positive for syphilis during her antenatal checkup in the first trimester. She was asymptomatic. She said her only sexual partner was her 60-year-old husband who had screened ‘negative’ for syphilis with his GP. She noted that her husband had become forgetful and irritable over the last year. I asked the patient’s husband to attend my clinic and performed both treponemal EIA and VDRL. The EIA was positive but VDRL was non-reactive. I subsequently performed lumbar puncture for her husband based on the suspicion of possible neurosyphilis. The CSF findings confirmed my suspicion! The first VDRL test performed by the GP was traced and was non-reactive. The patient’s husband was treated for neurosyphilis and had a good recovery.
|
3. A 30-year-old British male who had sex with males presented with a history of syphilis treated in my clinic 9 months prior. His post-treatment VDRL was 1:4. He complained of multiple small painful penile ulcers. He had unprotected oral sex 2 weeks prior to the consultation. I checked his RPR and performed herpes simplex virus (HSV) PCR for the ulcers: RPR was 1:4, treponemal EIA was positive and HSV PCR was negative. In view of the painful ulcers, I treated him empirically for genital herpes. I rechecked his RPR 2 weeks after the first blood test and the result came back 1:32. Hence, he was treated as a case of primary syphilis.
LEARNING POINTS: 1. Primary syphilis can present with painful ulcers although, classically, chancre is painless.4 2. In early primary syphilis, the non-treponemal test can be non-reactive. Therefore, the test should be repeated if primary syphilis is likely. 3. A treponemal test is not useful in this case as the patient previously had syphilis. |
Take home messages
- In high-risk and high-prevalence groups, using a treponemal test as the initial test may be advantageous and may avoid missing some stages of disease. One should also have a low threshold for testing, especially among high-risk populations.
- When ordering tests, make sure that you know the uses and limitations of treponemal and non-treponemal tests and order the correct tests. Use of only one test may be insufficient for diagnosis since there may be a false positive or a negative result for a single test.
- A documented history of treatment is important when interpreting discordant test results. In my practice, patients are given a record of their treatment so that they can use the information to better communicate with future healthcare providers.
- Determine what stage of syphilis the patient has clinically and serologically and give appropriate treatment accordingly. Laboratory test results must be considered together with the clinical and geographical background of the patient.
- When a patient presents to you with suspected syphilis, make use of the precious chance to screen for other sexually transmitted infections, including HIV.
Acknowledgement: The author wishes to express great
appreciation to Dr John W. Simon MH for his precious
advice in preparation of this article.
A complete list of references can be downloaded from
www.SOPHYSICIANSHK.org
Forward from《Journal of the Society of Physicians of Hong Kong》