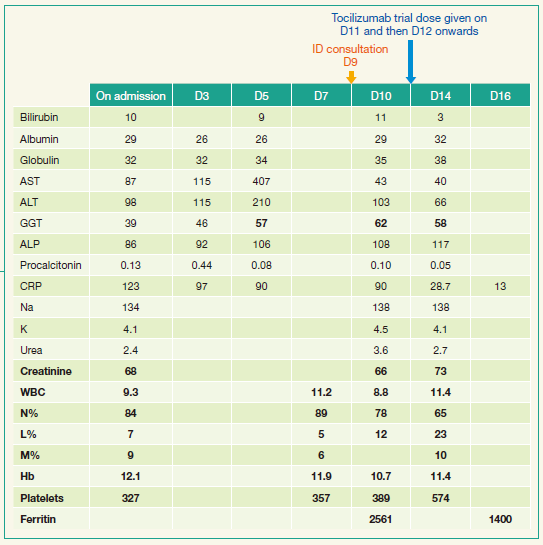
| Introduction I saw this 59 year old man at an in-patient consultation few months ago. He was the owner of a plastic toy company. He travelled 2 days a week to the countryside of Guangdong province where his factory was located. When he stayed at the factory, he consumed 2 raw egg yolks from his own chicken coop. He had no operations or serious illnesses. He took no regular medications. He had no allergies. He did not smoke and drank very little alcohol. He was married. His wife lived mainly in North Carolina where his children are in school. His appetite has been poor for the last few years. He now weighed 129lb and used to weigh 134-140lb. He gave a three-week history of a high swinging fever up to 39.7C. The below is an account of antibiotics that he had been given prior to seen by me. He was given Amoxil-clavulanate which he took for 3 days as an out-patient and was admitted and given Augmentin IV and Doxycycline 100mg bd orally. The Augmentin was changed to Meropenem 1g every 8 hours and doxycycline stopped 2 days later and changed to Azithromycin 500mg q24h IV which was changed to oral azithromycin 500mg daily. Gentamicin 60mg IV q8h was added 2 days later. His liver function had deteriorated since admission and he had been given Vitamin E 400mg bd. He had dysuria for two days before admission. He had a slight productive cough for a few days which disturbs him sleeping. Otherwise systemic enquiry did not reveal any other symptoms of note. On examination, there was no rash, eschar or lymphadenopathy. There is no neck stiffness and he is fully conscious and alert despite the fever. Examination of the cardiovascular system was normal and there was no murmur. There was no peripheral evidence of endocarditis. Chest auscultation revealed a few scattered crepitations and was otherwise normal. Abdominal examination showed no organomegaly. Rectal and genital examination were normal. Here is the basic haematology and biochemistry profile: |
| Review of Investigations CT low-dose thorax: linear atelectasis at lung bases CT abdomen & pelvis with & without contrast: prostate increased in size 47ml, 1cm renal cyst left kidney. Liver, spleen, pancreas all normal. Faecal loading of large bowel. Blood culture: no growth. It was repeated with extended culture time of at least 2 weeks and HACEK culture which eventually was negative. Urine microscopy: normal. MSU: no growth. Sputum grew Candida albicans. Nasopharyngeal swab and sputum respiratory PCR and Stool gastroenteritis PCR: all negative Hepatitis markers all negative: HBsAg negative, HBsAb positive, Hepatitis A IgG positive, HCV Ab negative The following tests were all negative: Quantiferon TB gold test , 1,3-beta-D-glucan , Malaria smear and antigen , Dengue screening ,Widal test, Melioidosis, Q fever, Lyme disease, Leptospiral and Rickettsial serology . EBV and CMV DNA. Mycoplasma IgM. ASOT. HIV 1&2 and p24Ag . INR was 1.3 ; APTT was 32 seconds. Thryoid function tests, LDH, calcium, phosphate and amylase were normal. |
| He was still running high swinging fever daily despite treatment for more than 1 week in hospital, but his general status was relatively well except fatigue. The rst day I saw him in hospital (D9 post admission), I decided to discontinue all his antibiotics. The next day I saw him, he told me that he had night sweats for a few days already. Subsequently, I have arranged an echocardiogram and PET-CT scan for him. Transthoracic echocardiogram showed possible vegetation on the tricuspid valve. There was thickened tricuspid valve chordal apparatus and a slender echogenic shadow. There was trivial tricuspid regurgitation. No pulmonary hypertension. Normal aortic valve trileaets. Normal mitral valve. Normal LV dimension and systolic function. Estimated ejection fraction 65-70%. Early left ventricular diastolic dysfunction. Right ventricle size was normal. PET-CT of the whole body including the brain showed no significant findings. Transoesophageal echocardiogram showed a 0.5cm mobile echogenic shadow attached to the chordal apparatus of septal leaets of tricuspid valve. Repeat Chest X ray showed no septic emboli. Because of dropping haemoglobin, stool was saved for occult blood and samples were negative. ESR came back 120 mm/hour. The Rheumatoid factor, ANA and ANCA were negative. Ig pattern was normal. Ferritin was 2561 and rechecked was 2510. Rheumatologist was consulted for suspected Adult onset Still’s disease. The patient was given a trial dose of Tocilizumab on D11 of his admission. All along he had no rash and joint pain, however, on the day after trial dose given, he was noticed to have mild ankle swelling of his left ankle and pinkish rash near to his left ankle which disappeared after a few hours.(Picture 1) That made the diagnosis of AOSD even more likely. He was put on full dose of Tocilizumab on D12 post admission and fever responded on the rst day. Thereafter he did not have further rash or joint pain. He was discharged on D16. All his blood culture on prolonged culture yielded no organisms. Repeat echocardiogram 3 months after discharge showed that the shadow was still there. |

| Final diagnosis: Adult onset Still disease (AOSD) Learning points: 1. Adult onset Still’s disease (AOSD) is very uncommon. A retrospective study estimated the annual incidence of AOSD to be 1.6 cases per 1 million people, with an equal distribution between the sexes[1]. 2. The diagnosis of AOSD is, in part, a diagnosis of exclusion. Look for characteristic clinical and laboratory features in the absence of another condition that may cause similar symptoms and findings. 3. The clinical presentation of AOSD is heterogeneous, but the most characteristic features are a. daily spiking fever; b. a cutaneous evanescent salmon-pink maculopapular eruption, most often present during the febrile hours; c. arthritis or arthralgia; d. leucocytosis with neutrophilia; e. a marked elevation in serum ferritin. 4. The classic skin rash of AOSD is usually non-pruritic and tend to occur with the fever and disappear when fever is gone. The rash occurs mainly on the trunk and extremities but can involve palm, sole and face. Hence it is important to regularly examine a patient with pyrexia of unknown origin for new signs. 5. Serum ferritin is elevated in as much as 70 percent of patients with AOSD. [2] The elevations correlate with disease activity and have been suggested as a serological marker to monitor response to treatment. Serum ferritin concentrations exceeding 3000 ng/mL (normal is 40 to 200 ng/mL) have been observed in AOSD, with some patients having values above 10,000 ng/mL [3] 6. In evaluation of patient with pyrexia of unknown origin, it is important to consider non-infectious causes. One has to exercise clinical judgement to stop empirical antibiotics and re-investigate when clinical features are not compatible with infections. Antibiotics are not without side effects as we see in this case. 7. Prior to June 2017, only 7 cases of AOSD-caused endocarditis were reported, among which left-sided valves (including aortic and bicuspid valves) were commonly involved.[4] Even so, it was challenging to confirm the existence of noninfective endocarditis in AOSD, especially the involvement of right-sided valves (mainly the tricuspid valve). The present case may be a case of AOSD-caused endocarditis. 8. Timely infectious disease consultation may help in patient management, reaching diagnosis earlier and improving patient outcome. It was found that among patients having sepsis, early ID consultation was associated with a 40% risk reduction for in-hospital mortality.[5] |
| References 1. Magadur-Joly G et al. Epidemiology of adult Still’s disease: estimate of the incidence by a retrospective study in west France. Ann Rheum Dis. 1995;54(7):587. 2. Ohta A et al. Adult Still’s disease: a multicenter survey of Japanese patients. J Rheumatol. 1990;17(8):1058. 3. Coffernils M et al. Hyperferritinemia in adult onset Still’s disease and the hemophagocytic syndrome.J Rheumatol. 1992;19(9):1425. 4. Dang X, Han Y and Zhang X. Endocarditis in Adult-onset Still Disease: A Case Report and Literature Review. J Rheumatol 2018; 45:1200-1201. 5. Madaline T et al. Early Infectious Disease Consultation Is Associated With Lower Mortality in Patients With Severe Sepsis or Septic Shock Who Complete the 3-Hour Sepsis Treatment Bundle. Open Forum Infectious Diseases 2019; 6 : ofz408 https://doi.org/10.1093/od/ofz408 |
Forward from《Union Hospital》